Study reveals shortcomings in how hospitals treat pain in children with sickle cell anaemia complication
A new study has found significant gaps in how hospitals in the UK comply with clinical guidelines when managing pain in children suffering from a complication linked to sickle cell anaemia.
The study 'Quality Improvement Project on the Pain Management of Vado-occlusive Crisis in Paediatric Patients with Sickle-cell Anaemia in Secondary Care ' will be presented at the Minoritised Life Scientists Future Forum which will be held in the ICC Birmingham this spring.
Samantha Monthe Taffou of Anglia Ruskin University who is presenting the study into pain management of vaso-occlusive crises (VOC) among children with sickle cell anaemia, said her findings highlight the need for systemic improvements in guideline adherence, education, and documentation to ensure equitable care. By addressing these gaps, healthcare providers can reduce unnecessary suffering, enhance patient trust, and improve overall efficiency in managing VOC cases.
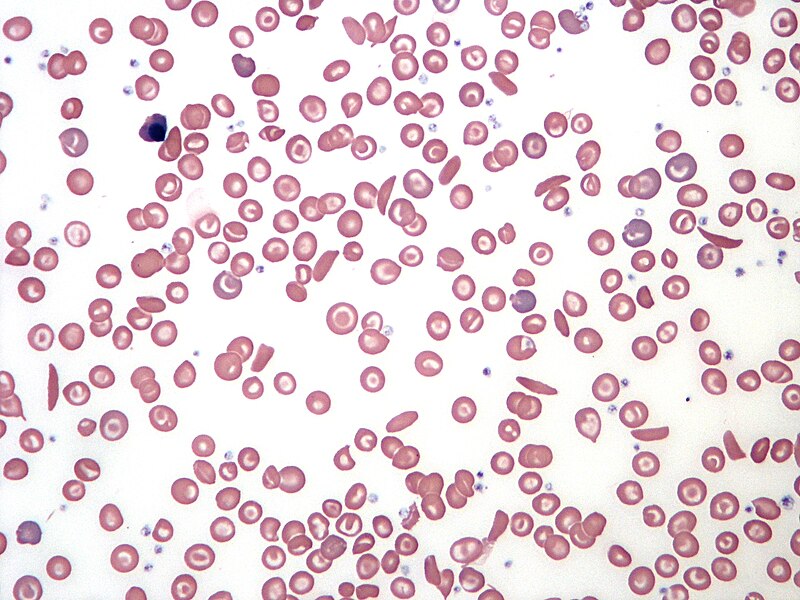
A vaso-occlusive crisis is a painful complication of sickle cell disease in which sickled red blood cells block small blood vessels, restricting blood flow to tissues and organs, causing severe pain due to tissue ischemia.
The Quality Improvement Project (QIP) undertaken by Miss Monthe Taffou investigated the pain management of vaso-occlusive crises (VOC) in paediatric sickle cell anaemia patients within a secondary care setting at an unnamed hospital.
Conducted in collaboration with the paediatric department, the study highlights significant gaps in compliance with national and local guidelines, particularly in the timely administration of analgesia and the use of pain-scoring tools.
“Sickle cell anaemia predominantly affects African-Caribbean populations, who often experience disparities in pain management due to racial bias, lack of clinician education, and systemic inefficiencies,” MIss Monthe Taffou said.
“National guidelines (NICE) recommend that patients receive analgesia within 30 minutes of presentation and that an age-appropriate pain-scoring tool be used. However, compliance remains inconsistent, leading to unnecessary patient suffering and potential complications. This project aimed to assess current practices at Hospital X, identify gaps, and propose interventions to enhance adherence to guidelines and improve patient outcomes.
“Given the critical nature of VOC, which can lead to severe pain, hospitalisation, and even early death, the findings offer valuable insights into healthcare disparities and practical interventions to improve patient care.”
The researchers conducted a clinical audit using the Plan-Do-Study-Act (PDSA) model. Data was collected from paediatric patients with VOC between 2020 and 2023, focusing on:
- The timeframe from initial assessment to administration of analgesia.
- The documentation and use of age-appropriate pain-scoring tools.
Findings revealed:
- 78% compliance in administering analgesia within 30 minutes.
- 67% compliance in documenting pain using age-appropriate pain-scoring tools.
- Lack of clarity in local guidelines contributed to inconsistencies in pain management.
- Clinicians were more likely to administer pain relief than to document pain scores correctly.
Proposed interventions include introducing electronic alerts for VOC patients; integration of pain-scoring tools and guidelines into digital hospital systems; gathering feedback from both staff and patients; and improved clinician education on VOC management.
One surprising finding was that despite the expectation that delays in analgesia administration would be a major issue, clinicians turned out to be more compliant in this aspect than in using pain-scoring tools. Additionally, some patients had pain assessed using inappropriate tools for their age, which could lead to underestimation of their pain and inadequate treatment.
Another unexpected finding was that local guidelines did not specify timeframes for initial analgesia administration like the national guidance, only for reassessment, contributing to documentation gaps and confusion among clinicians.
“Effective pain management in sickle cell VOC is essential to improving patient outcomes and reducing hospital admissions,” MIss Monthe Taffou said.
“The findings highlight the need for systemic improvements in guideline adherence, education, and documentation to ensure equitable care. By addressing these gaps, healthcare providers can reduce unnecessary suffering, enhance patient trust, and improve overall efficiency in managing VOC cases.”
To build on these findings, the following steps are recommended:
- Expanding the study to a larger sample size or multiple NHS institutions for broader applicability.
- Implementing the proposed interventions and reassessing their impact in a follow-up PDSA cycle.
- Exploring non-pharmacological approaches to pain management.
- Investigating the impact of clinician education on reducing racial bias in pain assessment and treatment.
- Conducting qualitative research on patient experiences to complement quantitative data.
This QIP was led by Samantha Monthe Taffou in collaboration with the Paediatric Department at Hospital X. The project was carried out as part of the MSc in Physician Associate Studies at Anglia Ruskin University. The hospital X QIP team provided consent and support for data collection, though time constraints prevented full implementation of interventions within this study period.
The Minoritised Life Sciences Future Forum conference (MLSFF) takes place from 31st March to 2nd April 2025 at the ICC Birmingham.
The final date to submit abstracts is 3 March 2025. To apply for a registration fee waiver and/or travel bursary you must apply for these before 28 February 2025. More details can be found here.
Caption: Blood smear illustrating sickle cell anaemia. Scooter Project, Keith Chambers

